Human Leukocyte Antigen (HLA): The Science Behind Stem Cell Compatibility
Successful stem cell transplantation depends not only on the quality of the cells but also on how well they are recognised by the recipient’s immune system. At the centre of this process is Human Leukocyte Antigen (HLA) - a set of genetic markers that help the body distinguish between its own cells and foreign ones, playing a key role in determining whether transplanted stem cells are accepted, function effectively, or trigger immune complications. At Cryoviva Life Sciences, stem cell preservation is viewed through the lens of transplant relevance and future medical applicability. By grounding preservation practices in established principles of immunology and HLA science, the focus extends beyond storage to safeguarding stem cells in a way that supports their potential usability as medical treatments continue to advance.
What is Human Leukocyte Antigen (HLA)?
Human Leukocyte Antigens (HLA) are proteins found on the surface of most cells in the body. They act as identification markers that help the immune system recognise which cells belong to the body and which are foreign. This recognition process is essential for protecting the body against infections while maintaining immune balance.
HLA markers are genetically inherited, with each person receiving one set from each parent. Because of this, HLA patterns tend to be similar among close family members, especially siblings. These inherited markers remain the same throughout life and play a central role in how the immune system responds to transplanted cells.
Why HLA Matching Matters in Stem Cell Transplants
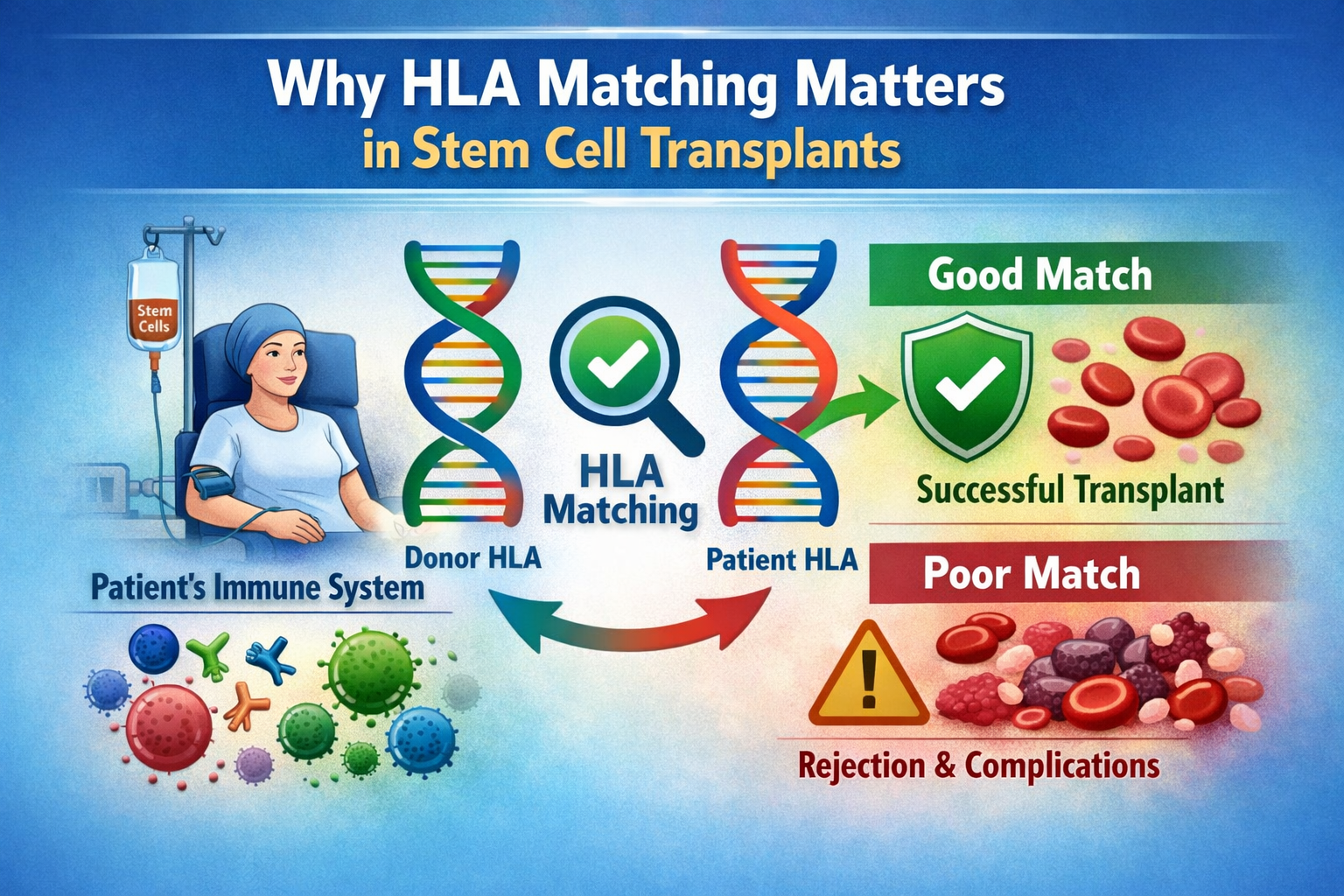
In stem cell transplantation, the immune system evaluates donor cells based on their HLA markers. When donor and recipient HLA profiles are closely matched, the transplanted stem cells are more likely to engraft successfully and perform their intended function within the body.
Poor HLA compatibility increases the risk of immune complications, making HLA matching a central factor in transplant planning for blood disorders, immune deficiencies, and certain cancers.
A good HLA match:
- Reduces the risk of graft rejection
- Lowers the likelihood of graft-versus-host disease (GVHD)
- Supports faster immune recovery after transplant
- Improves long-term treatment outcomes
Why Finding a Suitable Match Can Be Challenging
Because HLA markers are inherited, siblings are statistically the most likely to be good matches. However, many patients do not have access to a fully matched family donor, and finding a suitable unrelated donor can be time-consuming or uncertain.
In such situations, alternative stem cell sources become important. Umbilical cord blood stem cells are known for their greater immune tolerance, allowing successful transplantation even with partial HLA mismatches. This unique property has expanded transplant options for patients who might otherwise struggle to find compatible donors.
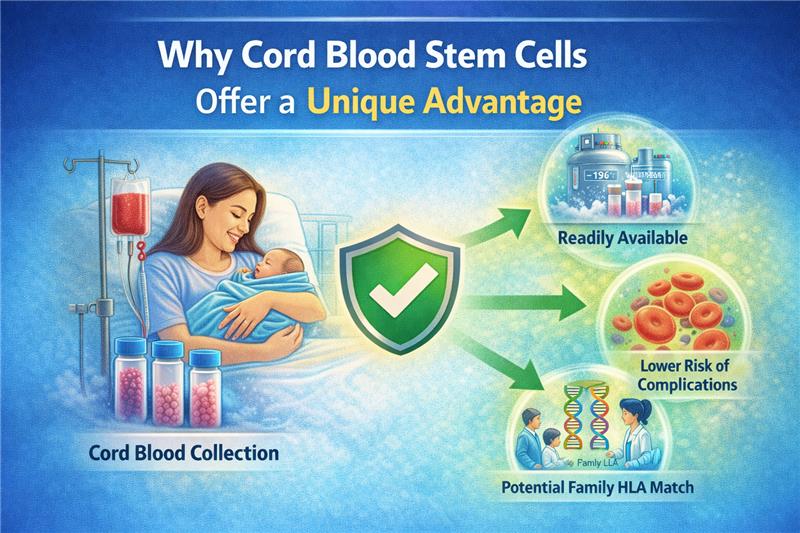
Why Cord Blood Stem Cells Offer a Unique Advantage
Umbilical cord blood is a rich and reliable source of stem cells that has become increasingly important in modern transplant medicine. Collected at birth, these cells offer distinct biological and clinical advantages that make them especially valuable for present and future medical use.
Unlike stem cells collected later in life, cord blood stem cells are preserved at the very beginning of life, before exposure to infections, environmental factors, or age-related cellular changes. This early preservation contributes to their unique therapeutic potential. Advantages include:
Biologically Younger and More Adaptable Cells
Cord blood stem cells are considered biologically immature, which allows them to adapt more easily when introduced into a recipient’s body. This flexibility supports better integration during treatment.
Key advantages include:
- Higher ability to develop into healthy blood and immune cells
- Lower risk of immune rejection compared to adult stem cells
- Greater tolerance for partial HLA mismatch in transplants
Reduced Risk of Immune-Related Complications
One of the major challenges in stem cell transplantation is immune incompatibility. Cord blood stem cells are less likely to trigger severe immune reactions, including graft-versus-host disease (GVHD), especially when compared to bone marrow or peripheral blood stem cells. This makes cord blood a valuable option when a fully matched donor is difficult to find.
Immediate Availability When Needed
Cord blood stem cells are collected once, at the time of birth, and can be cryopreserved for long-term storage. When required for treatment, they are readily available without the delays associated with donor searches or additional procedures. This immediate availability can be critical in time-sensitive medical conditions.
Expanding Role in Transplant and Regenerative Medicine
Cord blood stem cells are currently used in the treatment of various blood disorders, immune deficiencies, and certain cancers. Ongoing research continues to explore their potential in regenerative medicine, including neurological and metabolic conditions.
Preserving cord blood today helps families stay prepared for evolving treatment options in the future.
A Science-Backed Investment in Future Health
Cord blood banking is not just about storage; it is about safeguarding a biologically powerful resource at a time when it is at its highest quality. With growing advances in stem cell science, cord blood stem cells offer a unique advantage rooted in biology, compatibility, and long-term clinical relevance.
Family Matching and Future Treatment Possibilities

Stem cell compatibility is closely linked to genetics, which is why family members often provide the most suitable matches for transplantation. Human Leukocyte Antigen (HLA) markers are inherited, and siblings are more likely to share similar HLA profiles than unrelated individuals. This genetic connection makes family-based stem cell preservation an important consideration in long-term medical planning.
How Family Matching Works
Each child inherits half of their HLA markers from each parent. As a result:
- Siblings have a higher chance of being a close HLA match
- Parents may be partial matches for their children
- Preserved cord blood from one child may be suitable for a sibling or, in some cases, a parent
This shared genetic framework expands the potential usability of stored stem cells within the family.
Supporting Future Treatment Options
Preserving cord blood at birth creates a readily available stem cell source that may support future treatment needs. As transplant techniques and immunology-based therapies advance, the ability to access stem cells with known genetic and HLA profiles becomes increasingly valuable.
Potential future applications include:
- Treatment of blood and immune disorders within the family
- Support for evolving transplant protocols that allow partial HLA matches
- Integration into emerging therapies being explored through ongoing clinical research
Planning with Science and Preparedness
Family-based stem cell preservation is guided by medical principles rather than certainty of use. It reflects a proactive approach to healthcare - one that recognises genetic relationships, evolving medical science, and the importance of preparedness.
By aligning preservation decisions with HLA science and family matching potential, families can keep future treatment pathways open while relying on established transplant medicine foundations.
Cryoviva Life Sciences: Advancing Stem Cell Preservation Through HLA Science
At Cryoviva Life Sciences, stem cell preservation is guided by a deep understanding of transplant science and immune compatibility. Preservation is viewed not as storage alone, but as a long-term scientific commitment to maintaining the clinical relevance of stem cells as medical science continues to evolve. Central to this approach is Human Leukocyte Antigen (HLA) science, which plays a critical role in determining how stem cells may be used in future treatments.
By aligning preservation practices with established principles of immunology and transplant medicine, Cryoviva Life Sciences supports the potential usability of stored stem cells when advanced therapies may be required. Integrating HLA science into preservation planning reflects a commitment to responsible, future-ready healthcare - one that prioritises preparedness, clarity, and long-term value.
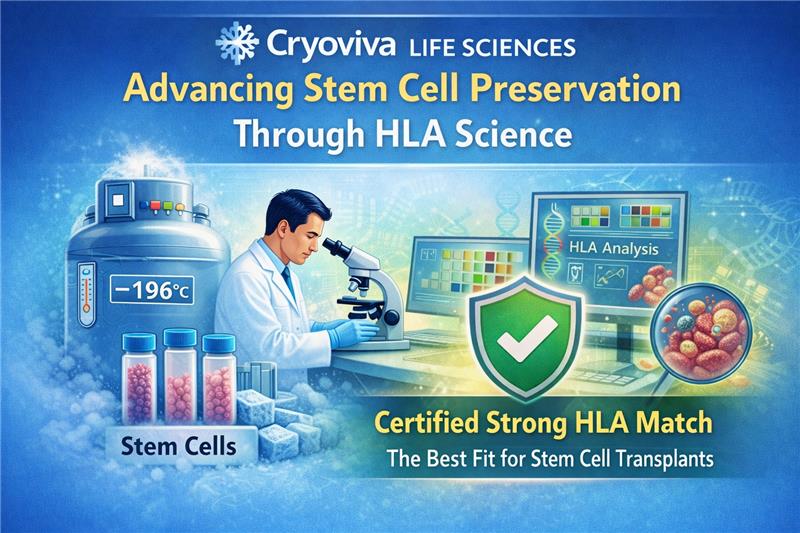
A Science-First, HLA-Informed Approach
Every stage of stem cell banking at Cryoviva Life Sciences follows a structured, science-driven framework designed to support immune compatibility and long-term clinical usability. Strong emphasis is placed on quality, consistency, and alignment with recognised scientific and regulatory standards.
This approach focuses on maintaining the integrity of preserved stem cells through stringent laboratory protocols, robust quality control measures, and preservation practices that support long-term viability. Processes are continually aligned with current transplant requirements and the evolving field of regenerative medicine.
Preparing for Tomorrow’s Transplant and Therapy Landscape
As transplant medicine advances, greater emphasis is being placed on precision matching, immune tolerance, and long-term treatment planning. Preserving stem cells with a clear understanding of HLA science helps ensure that families are better positioned for future medical needs; whether for established transplant indications or emerging therapeutic applications.
Through a disciplined, science-led approach, Cryoviva Life Sciences continues to advance stem cell preservation beyond storage, supporting informed decision-making and long-term clinical preparedness.
FREQUENTLY ASKED QUESTIONS
Is HLA the same as blood group matching?
No. Blood groups and HLA are different compatibility systems. Blood groups relate to red blood cells, while HLA markers are genetic identifiers present on most cells and play a key role in immune response and transplant compatibility.
Does everyone have a unique HLA type?
Yes. Each person has a unique combination of HLA markers inherited from their parents, which is why finding compatible donors can sometimes be challenging.
Why is HLA matching important even years after birth?
HLA markers do not change over time. Their relevance often emerges later in life if a stem cell or transplant-based treatment becomes necessary.
Are cord blood stem cells less strict about HLA matching?
Yes. Cord blood stem cells are more immunologically adaptable, allowing for successful transplants even when HLA matching is not exact.
Can stored stem cells be used for family members?
In some cases, yes. Because HLA markers are inherited, siblings and certain family members may share partial or close compatibility.
Is HLA testing done at the time of stem cell preservation?
HLA testing is typically performed when stem cells are being considered for clinical use, depending on the medical requirement and treatment plan.
Does a partial HLA match mean a transplant will fail?
Not necessarily. Advances in transplant medicine, particularly with cord blood stem cells, have made successful outcomes possible even with partial HLA matches.
How does understanding HLA help parents make informed decisions?
Awareness of HLA helps parents understand how genetic compatibility influences future treatment possibilities and why early stem cell preservation may hold long-term value.
Is HLA relevant only for transplants?
While HLA is most commonly associated with transplants, it also plays a role in immune-related research and the development of personalised medical therapies.
Will the importance of HLA increase in the future?
Yes. As regenerative medicine and personalised treatments continue to evolve, immune compatibility factors such as HLA are expected to become even more significant.
 Enquiry
Enquiry
 Email
Email Phone
Phone
 Whatsapp
Whatsapp